2. Center for Evidence-Based Medicine,Tianjin University of Traditional Chinese Medicine,Tianjin 300193,China.
Diminished ovarian reserve(DOR)refers to the condition of poor fertility which is characterized by limited numbers of remaining primordial follicles in the ovary and possibly impaired preantral oocyte development or recruitment(Wikipedia,2012).
Global prevalence of DOR is not studied largely because thus far the st and ard and agreed diagnostic criteria for it have not been defined. But it had been reported that merely 5% of women with evidence of DOR would achieve pregnancy,despite using of ovulation inducing agents(Scott et al,1995).
The exact causes for DOR have only been inadequately understood. The most common reason is advanced reproductive age(Gleicher et al,2011), and others include congenital(Skiadas et al,2012; Pastore et al,2012; Livshyts et al,2013),surgical(Biacchiardi et al,2011),medical causes(Clowse et al,2011),psychosocial stress(Pal et al,2010), and alcohol intake(Li et al,2013). Women confirmed of DOR diagnosis might present with infrequent menstruation,scanty periods,infertility,absence of menstrual bleeding,short follicular phase,or poor ovarian response to exogenous gonadotrophin at reproductive age(Loutradis et al,2007).
The current treatment strategies to address DOR have primarily focused on hormone replacement therapy to adjust the endocrine system and restore hormone balance. A few clinical studies showed some beneficial effects of dehydroepi and rosterone(DHEA)on DOR(Barad et al,2007; Gleicher et al,2009; Gleicher and Barad, 2011). However,its extensive use was not well-grounded and should be discouraged(Urman and Yakin, 2012). Traditional Chinese medicine(TCM)might provide a holistic approach and less harmful therapy to address the conditions of menstrual disorder or infertility affecting DOR patients.
The efficacy of TCM on patients with DOR has been tested in a few preliminary clinical studies with positive outcomes(Xu,2007). Moreover,both acupuncture and electro-acupuncture therapies have been reported to regulate the endocrine system(Cui et al,2007),stimulate ovulation(Yan and Huang, 1997), and improve ovarian blood flow(Stener-Victorin et al,2004)in women with DOR. Based on the current evidence,we conducted a systematic review and meta-analysis to examine the role of TCM in DOR,with special attention on TCM as an adjuvant to in vitro fertilization and embryo transfer(IVF-ET)in patients with DOR. 2. Methods 2.1 Inclusion criteria 2.1.1 Type of studies
Published r and omized controlled trials(RCTs)examing the role of various forms of TCM in treating women with DOR were eligible for inclusion. 2.1.2 Type of participants
Women of reproductive age with a serum level of follicle stimulating hormone(FSH)above 10 and below 40 IU/L. 2.1.3 Type of interventions
Intervention treatment with TCM therapeutic tools includes herbal medicine(HM),acupuncture(ACU),electro-acupuncture(EACU),moxibustion etc, and by alone or in the combination with Western medicine(WM)or IVF-ET or with them both as well. Treatment in the control group included placebo,no treatment,WM,IVF-ET,or combination of them. 2.1.4 Type of outcome measures
The primary outcomes were changes in basal serum FSH level and pregnancy rate(PR). The secondary outcomes were total effectiveness rate(TER),improvement in basal FSH/LH(luteinizing hormone)ratio,adverse events, and changes in basal serum E2 level,antral follicle count(AFC), and basal serum anti-Müllerian hormone level(AMH). We also compared the short-term(immediately after a 3-month treatment) and long-term(2 or 3 months after the last treatment)effects for one primary outcome and two secondary outcomes,namely changes in basal serum FSH level,improvement in FSH/LH ratio, and TER. Special attention was also paid to the role of TCM therapies as an adjuvant to IVF-ET. 2.2 Exclusion criteria
We excluded studies in which DOR was induced by unilateral or bilateral ovary removal surgery or participants included were diagnosed with premature ovarian failure(POF). Studies with unclear diagnostic criteria or without full texts were also considered ineligible for this review. 2.3 Search strategies
A comprehensive literature search was conducted in January 2013 in three English and five Chinese electronic databases including the Cochrane Central Register of Controlled Trials(CENTRAL,Issue 12,2012),EMBASE(1974.1–2013.1),PubMed(1966.1–2013.1),China National Knowledge Infrastructure(1956.1–2013.1),WanFang Database(1982.1–2013.1),VIP Database(1989.1–2013.1),Chinese Biomedical Database(CBM,1978.1–2013.1), and Chinese Clinical Trial Register(ChiCTR). The search strategy was formulated using MeSH terms in combination with free text words. The following is the search strategy developed for PubMed:
1. ovarian(text word,tw)
2. complementary medicine [Mesh terms]
3. acupuncture therapy [Mesh terms]
4. acupuncture [tw]
5. electroacupuncture [tw]
6. moxibustion [tw]
7. traditional Chinese medicine [Mesh terms]
8. Chinese medicine [tw]
9. herbal drug [tw]
1 0. herbal formula [tw]
1 1. herbal preparation [tw]
1 2. herbal medicine [tw]
1 3. Chinese patent drug [tw]
1 4. Chinese patent medicine [tw]
1 5. 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14
1 6. 1 and 15
We also checked the reference lists of included studies and relevant review articles for possible identification of eligible trials. Conference proceedings on ovarian diseases and women infertility were manually retrieved and screened. 2.4 Study selections
Two reviewers independently undertook the afore- mentioned search. Studies identified from electronic searches were first screened and duplicates were eliminated. Evidently irrelevant studies were excluded after a first round of screening by reading the title and abstract of all articles. Then the full-texts of the remaining studies were retrieved and assessed against our predefined inclusion criteria. Advice from a third reviewer was sought whenever disagreement arose between the two researchers. 2.5 Data collection and management
Two researchers designed the data extraction sheet and independently abstracted data from individual studies. Information concerning the name of the first author,year of publication,number of participants in each group,median age of patients,experimental and comparison intervention,herbal ingredients or acupoints involved,course of treatment,outcome measurements as well as the methodological characteristics of the included clinical studies were collected and cross-checked. 2.6 Assessment of risk of bias in included studies
Two reviewers assessed the quality of included studies independently using the Cochrane risk of bias assessment tool(Higgins and Green, 2008)consisting of six domains. The results are summarized in Table 1. A judgment of “yes” will be made if the method of r and om sequence generation,allocation concealment or blinding were described,or no incomplete data,selective reporting and other sources of bias existed,suggesting low risk of bias for each item assessed. “Unclear” means no details on the production of r and om sequence and other five check items can be found in the original article. And “no” denotes that allocation concealment or blinding was not used,missing data existed and were not addressed,a selection of variables was recorded or that other sources of bias such as baseline imbalances existed,which is indicative of high risk of bias.
| Table 1 Summary of quality assessment of RCTs |
We used Review Manager 5.0.2,provided by the Cochrane collaborations,for data analysis. We assessed heterogeneity across trials to decide whether it is meaningful to have the data pooled by using the Chi-square test and I2 statistic with a significance level of 0.05. I2 < 50% means moderate heterogeneity and I2 > 50% means notable heterogeneity. In the former case,relative risk(RR)was calculated for dichotomous data and mean difference(MD)for continuous data,both using a fixed-effect model and with 95% confidence interval(CI). If substantial heterogeneity was detected as in the latter case(I2 > 50%),original studies were reviewed to check the data entered and identify possible causes. A r and om-effect model will be used if the variation could not be explained. Interpretation of pooled results using this model shall be done with care. 3. Results
A total of 6834 articles were identified through electronic searches. Two reviewers have read the title and abstract of these studies and excluded apparently irrelevant articles and non-clinical studies. After initial screening,369 articles were left. The full-texts of these articles were then retrieved and checked against the inclusion criteria. Finally,17 studies(Arnoldi et al,2010; Chen,2011a; Chen,2011b; Fu et al,2011; Li,2004; Li and Guo, 2008; Li et al,2011; Liu,2008; Liu,2012; Lv,2011; Wang,2008; Wang,2012; Wang et al,2012; Xu et al,2009; Zhang,2010; Zhong,2011; Zhu,2012)were included,16 in Chinese and 1 in English(Figure 1).
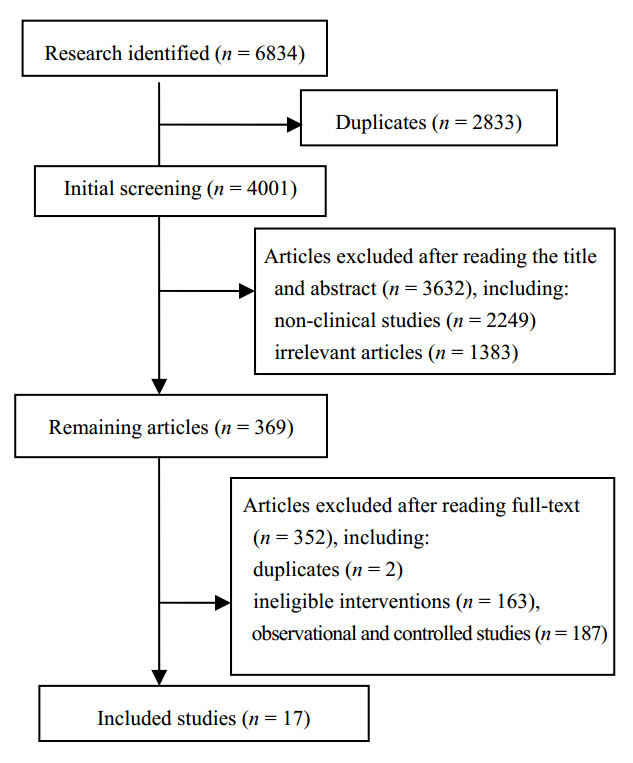 | Figure 1 Flow diagram of study selection |
A total of 17 RCTs involving 1174 patients were analyzed in this review. Sample size ranged from 34 to 178. Treatment course was 3 months in 13 trials,6 months in one study, and not reported in three articles. We categorized the 17 studies into eight subgroups based on the type of intervention and comparison. Among them,10 studies compared HM with WM,one study compared HM plus WM with WM(Liu,2012), and the other six examined the role of TCM(HM,Acu,Eacu,TEAS, and acronym for transcutanclus electrical acupoint stimulation,or combined therapy)in IVF-ET. Details on the intervention and control treatment of included RCTs were specified below:
1. 10 HM vs WM
2. 1 HM + WM vs WM
3. 1 HM + IVF-ET vs IVF-ET
4. 1 Acu + IVF-ET vs IVF-ET
5. 1 Eacu + IVF-ET vs IVF-ET
6. 1 TEAS + IVF-ET vs IVF-ET
7. 1 TEAS + HM + IVF-ET vs IVF-ET
8. 1 TEAS+ WM + IVF-ET vs WM +IVF-ET
HM interventions included herbal decoction(eight studies),Chinese patent drugs(CPD,two studies), and granular formulation(three studies). WM included estrogen,progestin,DHEA, and estrogen-progestin combinations. More details could be found in Tables 2 and 3.
| Table 2General characteristic of included studies |
| Table 3 General characteristic of included studies |
All 17 articles mentioned the word “r and omization”,but only seven studies(Chen,2011b; Li and Guo, 2008; Li et al,2011; Lv,2011; Wang,2012; Wang et al,2012; Zhong,2011)elaborated on the method used. Six of them used r and om number table, and the other studies(Wang,2012)used computer-generated r and om sequence. None mentioned allocation concealment. Only one study(Wang,2008)mentioned the performance of single blinding.
Reporting of incomplete outcome data was observed in six studies. Among them one study(Wang,2012)reported that missing data did not cause imbalances among groups. In another study(Arnoldi et al,2010),data loss was due to that six participants in the experiment and 20 in the control group did not receive embryo transfer,leading to inter-group statistical significance(P < 0.01). In two trials(Wang et al,2012; Chen,2011a),five and three patients had natural pregnancy during the treatment,respectively. In the remaining two trials,a few participants withdrew because they were considered ineligible for controlled ovarian hyperstimulation(COH),involving three patients in the treatment and six in the control group in one study(Zhu,2012) and five patients in the treatment and 11 in the control group for another one(Zhang,2010).
Two studies reported a selection of outcomes(Arnoldi et al,2010; Wang et al,2012). With regards to other biases,15 studies involved the use of self-prepared and individualized herbal decoction or granular formulation according to the doctor’s prescription. All included trials compared with the treatment and control groups at baseline to ensure that they were comparable. 3.3 Effects of interventions 3.3.1 Basal serum FSH level
A total of 14 trials reported changes in basal serum FSH level over a 3-month treatment. Data in one study(Fu et al,2011)with a treatment course of 6 months was inconsistent and therefore not used in the pooled analysis.
1 )HM vs WM
Seven trials reported the changes of basal serum FSH level at the end of treatment. Pooled analysis showed that the FSH level in patients receiving HM was 1.7 IU/L lower compared with WM(MD = −1.70,95% CI = −2.63 to −0.77; P = 0.16,I2 = 35%).
2 )HM vs WM(baseline vs 2 months after treatment ended)
Two studies measured the basal serum FSH level at baseline and in months after the treatment ended. Patients in the TCM group experienced a greater reduction of FSH levels compared with the patients in the WM group(MD = −4.60,95% CI = −6.26 to −2.90; P = 0.34,I2 = 0).
3 )HM vs WM(baseline vs 3 months after treatment ended)
Two studies compared the basal serum FSH level at baseline with that in months after the treatment ended. Similarly,patients in the TCM group experienced a greater reduction of FSH levels compared with the patients in the WM group(MD = −4.47,95% CI = −6.56 to −2.39). However,a r and om-effect model was used because notable hetero- geneity was evident in this analysis(P = 0.02,I2 = 81%).
Results of subgroup meta-analysis indicated further reduced FSH level in 2 or 3 months after the treatment ended than immediately after the treatment(MD = −4.60/−4.47 vs MD = −1.70),as shown in Figure 2.
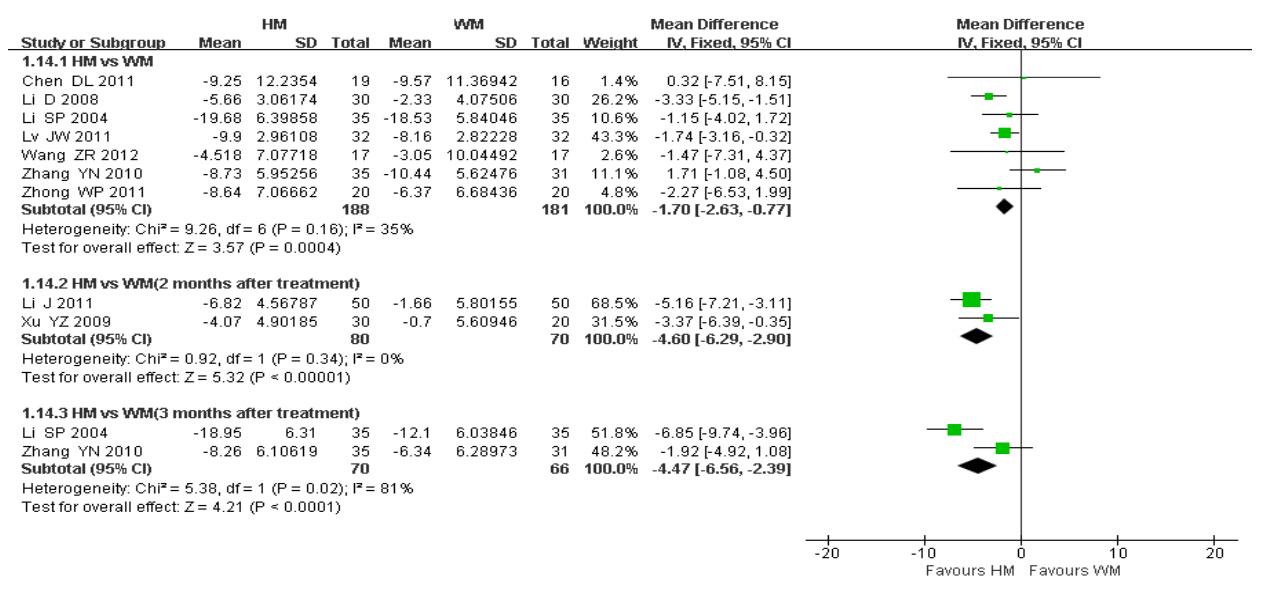 | Figure 2 Changes in basal serum FSH levels |
Seven trials reported the PR of participants.
1 )Role of TCM in IVF-ET
Five trials investigated the effects of various TCM modalities on DOR patients undergoing IVF-ET. Because each of these trials had a specific type of intervention and comparison,we first examined the relative effects for this outcome in each study one by one, and then assessed the effect in a pooled analysis.
AFC: antral follicle count; AMH: anti-Müllerian hormone; C: control group; CT: course of treatment; DHEA: dehydroepi and rosterone; Eacu: electropuncture; E2: estradiol; Em: endometrium; FSH: follicle-stimulating hormone; FN: follicle count; INHB: inhibin B; IVF-ET: in vitro fertilization and embryo transfer; IVF-ET Ps: IVF-ET stimulation,laboratory and embryo transfer parameters; KI: kuppermann index; LH: luteinizing hormone; MP: improvement in menstrual pattern; NA: not available; OV: ovarian volume; OVD: ovarian diameter; PR: pregnancy rate; PI: pulsatility index; PSV: peak systolic velocities; RI: resistance index; S/D: systolic/diastolic velocity ratio; TCMSS: traditional Chinese medicine symptom score; T: treatment group; TI: intervention in treatment group; TEAS: transcutanclus electrical acupoint stimulation; TER: total effective rate
As being seen in Figure 3,no statistically significant difference in PR was observed between the TCM + IVF-ET and IVF-ET groups for each specific type of intervention and comparison. However,pooled analysis of the five studies showed the odds of achieving pregnancy with TCM therapy as an adjuvant to IVF-ET were 1.75 folds greater than those with IVF-ET alone in women with DOR(RR = 1.75,95% CI = 1.25 to 2.46; P = 0.001,I2 = 0).
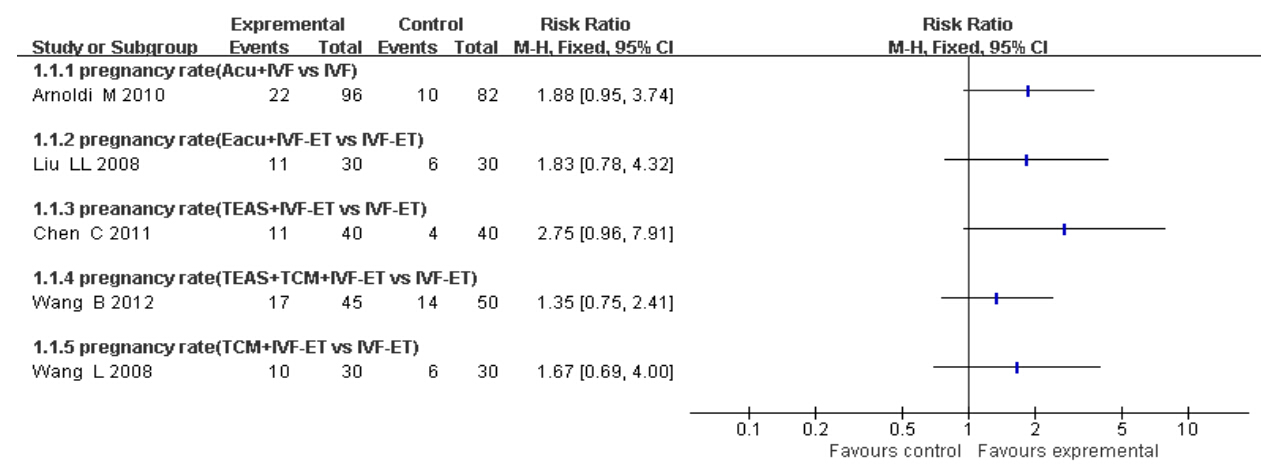 | Figure 3 PR of each woman |
2 )HM vs WM
In one trial(Wang,2012),no statistical difference in PR was observed between the HM and WM groups(P = 0.38).
3 )TEAS+WM+IVF-ET vs WM+IVF-ET
In another study(Zhu,2012),no statistical difference in PR was observed between patients receiving TEAS in combination with WM and IVF-ET and patients treated with WM and IVF-ET(P = 0.07). 3.3.3 FSH/LH ratios
Five trials reported the ratios of FSH/LH.
1 )HM vs WM
Three trials(Li and Guo, 2008; Lv,2011; Wang,2012)reported the ratio of FSH/LH and compared the ratio calculated at baseline with that at the last visit. Meta-analysis using fixed-effect model revealed patients taking HM had far lower FSH/LH ratios than those having WM(MD = −0.43,95% CI = −0.56 to −0.30; P = 0.53,I2 = 0).
2 )HM vs WM(baseline vs two months after the treatment ended)
Another two trials(Li et al,2011; Xu et al,2009)reported the outcome and compared the ratio calculated at baseline with those two months after the treatment ended. The ratio of FSH/LH in the HM group was notably decreased compared with that in the WM group(MD = −0.56,95% CI = −0.85 to −0.28; P = 0.63,I2 = 0%).
Results of subgroup meta-analysis indicated further decreased FSH/LH ratios in 2 months after the treatment ended compared with immediately after the treatment,as evident in Figure 4.
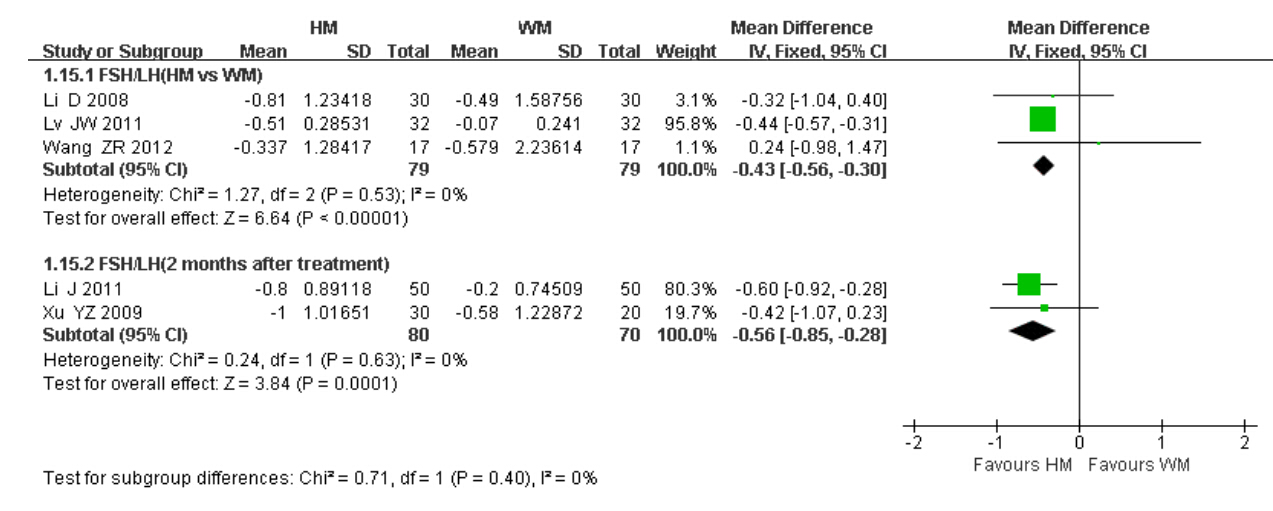 | Figure 4 FSH/LH ratios |
Six trials reported the changes in basal serum LH level.
1 )HM vs WM
Five trials reported changes in the basal serum LH level over a 3-month treatment period. Meta-analysis showed that no statistical difference existed between the two groups(MD = −0.06,95% CI = −0.33 to 0.22; P = 0.42,I2 = 0%)(Figure 5).
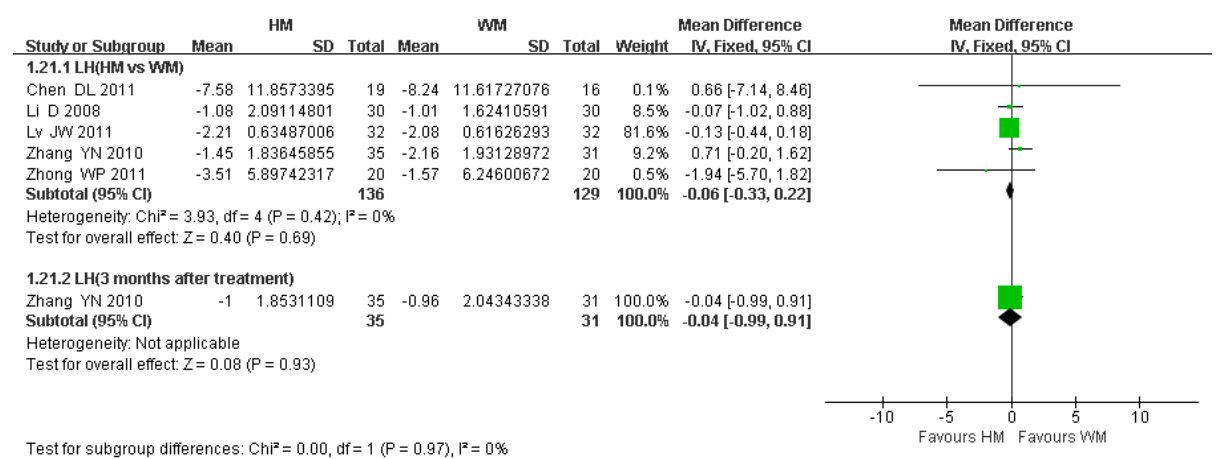 | Figure 5 Basal serum LH level |
2 )HM vs WM(baseline vs 3 months after treatment ended)
One trial(Zhang,2010)compared the basal serum LH level at baseline with that of 3 months after the treatment ended. Also,no statistical difference was found between the two groups(P = 0.93). 3.3.5 Total effective rates
1 )HM vs WM
Eight trials reported the total effective rates of HM vs WM for the management of DOR. Pooled analysis using the r and om-effect model found no statistical differences in the effects between the two groups(P = 0.30; P = 0.0005,I2 = 73%). The notable variation across the trials can be explained by the high risk of bias generally involved in studies and varied st and ards by which whether the treatment is “effective” in individual trials could be judged(Figure 6).
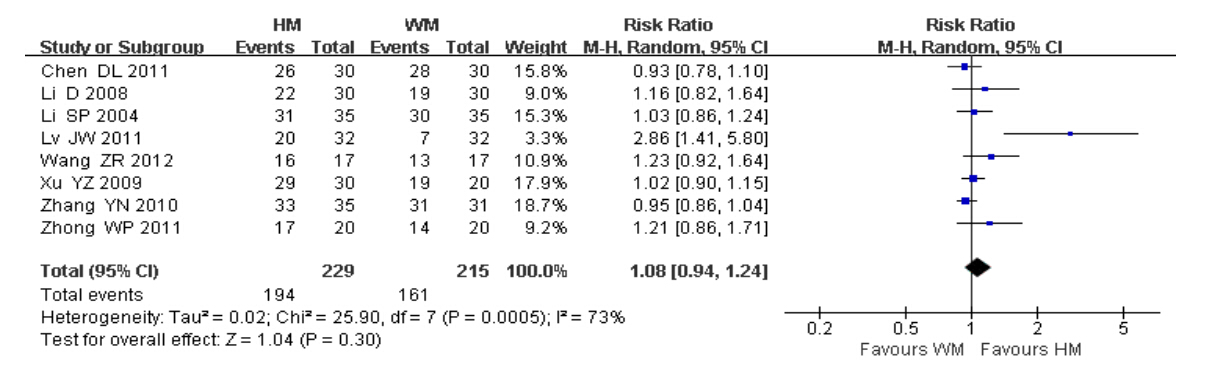 | Figure 6 Total effective rate |
2 )HM vs WM(2 months after the treatment ended)
Two trials did not measure the total effective rates immediately after treatment,but 2 months after the treatment ended. In a pooled analysis of the two trials the total effective rate was higher in participants having HM compared to those with WM(PR = 1.93,95% CI = 1.48 to 2.52; P = 0.18,I2 = 43%). 3.3.6 AFC
1 )HM vs WM
Changes in AFC were reported in three trials. Pooled analysis revealed AFC was mildly greater in patients receiving HM compared to those receiving WM(MD = 0.44,95% CI = 0.04 to 0.83; P = 0.61,I2 = 0%),but the measure has a broad CI. 3.4 Sensitivity analysis
We conducted a sensitivity analysis for the two primary outcomes by comparing fixed and r and om-effect estimates or by excluding the studies with distinguished features from the meta-analysis. For FSH level,pooling data of the seven trials comparing HM with WM yielded(MD = −1.70,95% CI = −2.63 to −0.77)in the fixed-effect model,compared with MD −1.49(95% CI −2.83 to −0.15)using the r and om-effect model. Sensitivity analysis excluding the trial(Lv,2011)by highly prone to selection bias resulted in an MD of −1.67(95% CI = −2.91 to −0.43). With regards to PR,sensitivity analysis including all seven trials reporting the outcome(regardless of intervention types)resulted in a RR of 1.85(95% CI = 1.34 to 2.55)with the fixed-effect model and a RR of 1.79(95% CI = 1.30 to 2.47)with the r and om-effect model. Sensitivity of five trials excluding two significant studies(Arnoldi et al,2010; Wang et al,2012)weighting a little more than 50% when combined yielded a PR of 2.14(95% CI 1.35 to 3.40). 3.5 Safety analysis
Five of the 17 trials reported the occurrence of adverse events. In one study(Liu,2012),nausea and vomiting,abdominal distension or swollen breasts were observed in four cases in the WM group and one case in the HM plus WM group. One trial(Chen,2011b)reported five cases of stomach discomfort and three cases of swollen aching breast in patients receiving HM compared to seven cases of stomach comfort and six cases of swollen aching breast in patients with WM. Also,one patient in the WM group had elevated glutamic oxaloacetic transaminase(GOT) and guanosine triphosphate(GTP)levels in liver function test,which disappeared soon after the treatment ceased. In another study(Zhang,2010),one patient in the HM group had diarrhea, and three patients in the WM group had nausea and one had stomache. In two studies(Chen,2011a; Zhong,2011)no adverse events were observed in either group.
The publication bias was also assessed and funnel plot was made according to the data of basal serum FSH level reported in 14 included studies(Figure 7). The results show that a potential publication bias exists. The possible reason is that most of included studies were conducted in China and published in Chinese, and language bias and geographical bias were caused.
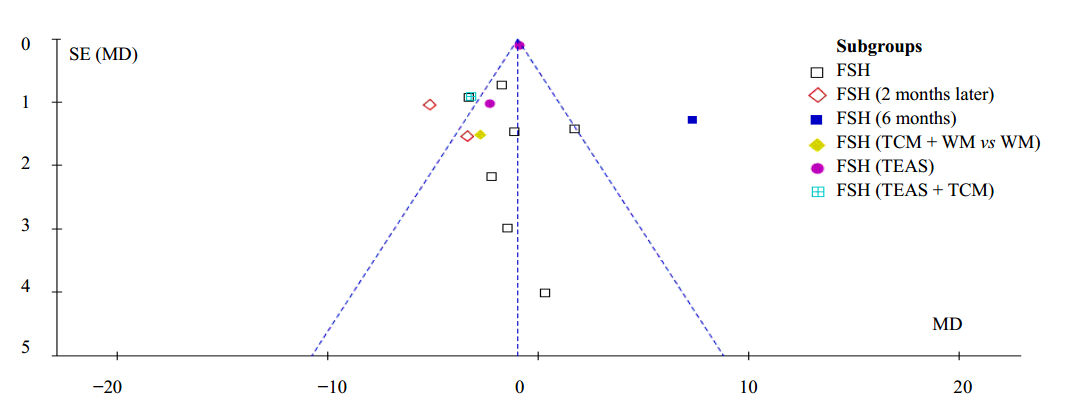 | Figure 7 Funnel plot |
This systematic review found HM was superior to WM in reducing basal serum FSH level(MD = −1.70) and the ratio of FSH to LH(MD = −0.43), and the effect was more evident 2 months after the treatment ended(MD = −4.60 for FSH and MD = −0.56 for FSH/LH). These extra 2 or 3 months would be the golden time for patients holding a “childbirth” wish to receive IVF or other types of ART. HM was also proved better for increasing AFC compared with WM(MD = 0.44).
Despite continuous efforts to develop and improve ART in the recent decade,the live birth rate even for women with normal ovarian reserve(NOR)remained unsatisfactorily low(an average of 20% to 30% cycles would be successful)(Maheshwari et al,2006; Gunby et al,2011). For women with DOR,only 15% of ART cycles would result in live births(CDC,2013). Repeated and failed IVF-ET cycles inflicted heavy emotional and financial burden on the couples. For females,especially,controlled ovarian hyperstimulation may induce serious side effects such as ovarian enlargement,ovarian hyperstimulation syndrome, and others. In this review,we found TCM could be a promising complementary therapy for the patients undergoing IVF-ET,in that the odds of achieving pregnancy with TCM was 1.75 folds greater compared to those of blank in IVF-ET. Besides the evidence on efficacy,a summary of reports of adverse events indicating the various modalities of TCM had a good safety profile.
According to a comprehensive literature search,this is the first systematic review of TCM for DOR. Our findings suggest herbal medicine,acupuncture and /or other TCM modalities can help restore reproductive hormone balance,improve reproductive capacity, and enhance the success rate of IVF-ET. 5. Limitations
A consensus on the definite diagnosis of DOR has not been reached. The majority of the included studies was conducted in China,with only one in Italy. The inclusion of data form unpublished, and other grey literature was not considered. The sample sizes of the present trials were quite small. Varied modalities of TCM have been included in the analysis,which can in part explain the heterogeneity amongst trials. Trials included in this review are considered to be of moderate to low quality. Consequently,the conclusions drawn are far from conclusive.
| [1] | Arnoldi M, Diaferia D, Corbucci MG, De Lauretis L, 2010. The role of acupuncture in patients at unfavourable reproductive prognosis in IVF: A prospective r and omised study; Abstracts of the 26th Annual Meeting of ESHRE; 2010 June 27-30 Italy, the 26th Annual Meeting of ESHRE; Rome, i257 |
| [2] | Barad D, Brill H, Gleicher N, 2007. Update on the use of dehydroepi and rosterone supplementation among women with diminished ovarian function. J Assist Reprod Gene 24(12): 629-634. |
| [3] | Biacchiardi CP, Piane LD, Camanni M, Deltetto F, Delpiano EM, Marchino GL, Gennarelli G, Revelli A, 2011. Laparoscopic stripping of endometriomas negatively affects ovarian follicular reserve even if performed by experienced surgeons. Reprod Biomed Online 23(6): 740-746. |
| [4] | CDC, 2013. ART 2010 National Summary Report; Section 2: ART Cycles Using Fresh, Nondonor Eggs or Embryos(Part B). Available from: URL: http://www.cdc.gov/art/ART2010/ sect2_fig16-26.htm#f19 |
| [5] | Chen C, 2011a. Study of the effect of transcutanclus electrical acupoint stimulation intervene in the patients with ovarian poor respond. Sh and ong University of TCM. |
| [6] | Chen DL, 2011b. Clinical study on the effect of Kuntai capsule on decreasing ovarian reserve and premature ovarian failure. Hubei University of TCM. |
| [7] | Clowse ME, Copl and SC, Hsieh TC, Chow SC, Hoffman GS, Merkel PA, Spiera RF, Davis JC Jr, McCune WJ, Ytterberg SR, St Clair EW, Allen NB, Specks U, Stone JH; WGET Research Group, 2011. Ovarian reserve diminished by oral cyclo- phosphamide therapy for granulomatosis with polyangiitis(Wegener’s). Arthritis Care Res(Hoboken) 63(12): 1777-1781. |
| [8] | Cui W, Sun W, Liu LL, Wen J, 2007. Investigation on effect of electroacupuncture intervention on in vitro fertilization and embryo transfer patients. Matern Child Health Care China 22: 3403-3405. |
| [9] | Fu XH, Li Q, Zhu SL, Chang YN, Tian XN, Chen HH, Zhang BJ, 2011. Bu Shen Huo Xue Prescription in the treatment of 27 cases of hypomenorrhea after induced abortion. Modern TCM 31(3): 26-28. |
| [10] | Gleicher N, Barad D, 2011. Dehydroepi and rosterone(DHEA)supplementation in diminished ovarian reserve(DOR). Reprod Biol Endocrinol 9: 67. |
| [11] | Gleicher N, Ryan E, Weghofer A, Blanco-Mejia S, Barad DH, 2009.Miscarriage rates after dehydroepi and rosterone(DHEA)supplementation in women with diminished ovarian reserve: A case control study. Reprod Biol Endocrinol 7: 108. |
| [12] | Gleicher N, Weghofer A, Barad DH, 2011. Defining ovarian reserve to better underst and ovarian aging. Reprod Biol Endocrinol 9: 23. |
| [13] | Gunby J, Bissonnette F, Librach C, Cowan L; IVF Directors Group of the Canadian Fertility and Andrology Society, 2011. Assisted reproductive technologies(ART)in Canada: 2007 results from the Canadian ART register. Fertil Steril 95(2): 542-547. |
| [14] | Higgins JTP, Green S, 2009. Cochrane h and book for systematic reviews of interventions. Version 5.0.2, (updated September 2009). The Cochrane Collaboration, 2009. Available from http://www.cochrane-h and book.org [accessed 7 June 2011]. |
| [15] | Li D, Guo J, 2008. Application of kidney-reinforcing and menstrual cycle-regulating therapy in assisted reproductive techniques for improving ovarian reserve. J Beijing Univ TCM 31(2): 131-134. |
| [16] | Li J, Zheng J, Chen YC, Ni S, Gao J, Wu RX, 2011. Effect of replenish kidney and activate bloodtreatment for 50 women with diminished ovarian reserve. Chin J Integr Med 31(10): 1429-1430. |
| [17] | Li N, Fu S, Zhu F, Deng X, Shi X, 2013. Alcohol intake induces diminished ovarian reserve in childbearing age women. J Obstet Gynaecol Res 39(2): 516-521. |
| [18] | Li SP, 2004. Effect of nourishing kidney and clear liver treatment for 35 women with diminished ovarian reserve. J Sichuan TCM 22(12): 62-63. |
| [19] | Liu LL, 2008. Study of the effect of electro-acupuncture treatment on oocyte quality and outcome of the patients undergoing in-vitro-fertilization and embryo transfer. Sh and ong University of TCM. |
| [20] | Liu LL, 2012. Clinical study on treating oligomenorrhea of low ovarian reserve function with Zishentang combined with western medicine artificial cycle. Heilongjiang University of TCM. |
| [21] | Livshyts G, Podlesnaja S, Kravchenko S, Livshits L, 2013. Association of PvuII polymorphism in ESR1 gene with impaired ovarian reserve in patients from Ukraine. Reprod Biol 13(1): 96-99. |
| [22] | Loutradis D, Drakakis P, Vomvolaki E, Antsaklis A, 2007. Different ovarian stimulation protocols for women with diminished ovarian reserve. J Assiste Reprod Genet 24(12): 597-611. |
| [23] | Lv JW, 2011. Clinical effect of replenish kidney and clear the heart treatment for women with diminished ovarian reserve. Guangming J Chin Med 26(9): 1806-1807. |
| [24] | Maheshwari A, Fowler P, Bhattacharya S, 2006. Assessment of ovarian reserve−Should we perform tests of ovarian reserve routinely? Hum Reprod 21(11): 2729-2735. |
| [25] | Pal L, Bevilacqua K, Santoro NF, 2010. Chronic psychosocial stressors are detrimental to ovarian reserve: A study of infertile women. J Psychosom Obstet Gynaecol 31(3): 130-139. |
| [26] | Pastore LM, Young SL, Baker VL, Karns LB, Williams CD, Silverman LM, 2012. Elevated prevalence of 35-44 FMR1 trinucleotide repeats in women with diminished ovarian reserve. Reprod Sci 19(11): 1226-1231. |
| [27] | Scott RT, Opsahl MS, Leonardi MR, Neall GS, Illions EH, Navot D, 1995. Life table analysis of pregnancy rates in a general infertility population relative to ovarian reserve and patient age. Hum Reprod 10(7): 1706-1710. |
| [28] | Skiadas CC, Duan S, Correll M. Rubio R, Karaca N, Ginsburg ES, Quackenbush J, Racowsky C, 2012. Ovarian reserve status in young women is associated with altered gene expression in membrana granulosa cells. Mol Hum Reprod 18(7): 362-271. |
| [29] | Stener-Victorin E, Kobayashi R, Watanabe O, Lundeberg T, Kurosawa M, 2004. Effects of electro-acupuncture stimulation of different frequencies and intensities on ovarian blood flow in anaesthetized rats with steroid−induced polycystic ovaries. Reprod Biol Endocrinol 2: 16. |
| [30] | Urman B, Yakin K, 2012. Does dehydroepi and rosterone have any benefit in fertility treatment? Curr Opin Obstet Gynecol 24(3): 132-135. |
| [31] | Wang B, Chen C, Wang YN, Xing GG, Sun W, 2012. Therapeutic effect of Wenshen Yangxue Granule combined with transcutanclus electrical acupoint stimulation on treatment of patients with poor ovarian response in IVF−ET. Chin J Hum Sexuality 21(5): 32-35. |
| [32] | Wang L, 2008. Studies on the mechanism of shen qi deficiency of senile infertile women undergoing IVF-ET and therapeutic evaluation of Erzhi Tiangui Granules. Sh and ong University of TCM. |
| [33] | Wang ZR, 2012. Clinical research on effect of kidney-tonilying Traditional Chinese Herbs to improve the female reproductive potential in late-reproductive age. Guangzhou University of TCM. |
| [34] | Wikipedia, 2012. Poor ovarian reserve. Available from: URL: http://en.wikipedia.org/wiki/Poor_ovarian_reserve. |
| [35] | Xu QC, 2007. Clinical studies on tonifying kidney herb in improving the ovarian reserve of the sterility women. Sh and ong University of TCM. |
| [36] | Xu YZ, Dong MX, Zhao L, 2009. Effect of replenish the kidney essence for 30 women with diminished ovarian reserve. Shanxi J TCM 30(11): 1445-1446. |
| [37] | Yan M, Huang YJ, 1997. Clinical effective analysis of 83 cases of electroacupuncture ovulation. Chin Acupunct Moxib 16(11): 651-652. |
| [38] | Zhang YN, 2010. The clinical observing of bu shen shu gan method for improving decreasing ovarian reserve. Heilongjiang University of TCM. |
| [39] | Zhong WP, 2011. Clinical study of bu-shen-huo-xue decoction on treating decreased ovarian reserve on account of psychological stress. Nanjing University of TCM. |
| [40] | Zhu N, 2012. Study of the effect of transcutanclus electrical acupoint stimulation to the patients with ovarian poor response in the effect of pregnancy outcome. Sh and ong University of TCM. |
 2014, Vol. 6
2014, Vol. 6


